BJS Academy>Continuing surgical ...>BJS sample document ...
BJS sample document- test
Velde G, Ismail W, Thorsen K.
Br J Surg 2024; 111: znae224.
12 November 2025
Upper GI
Related articles
The management of oesophageal cancer: the surgeon’s perspective
Eider Talavera-Urquijo, MD PhD, Bas P. L. Wijnhoven, MD PhD
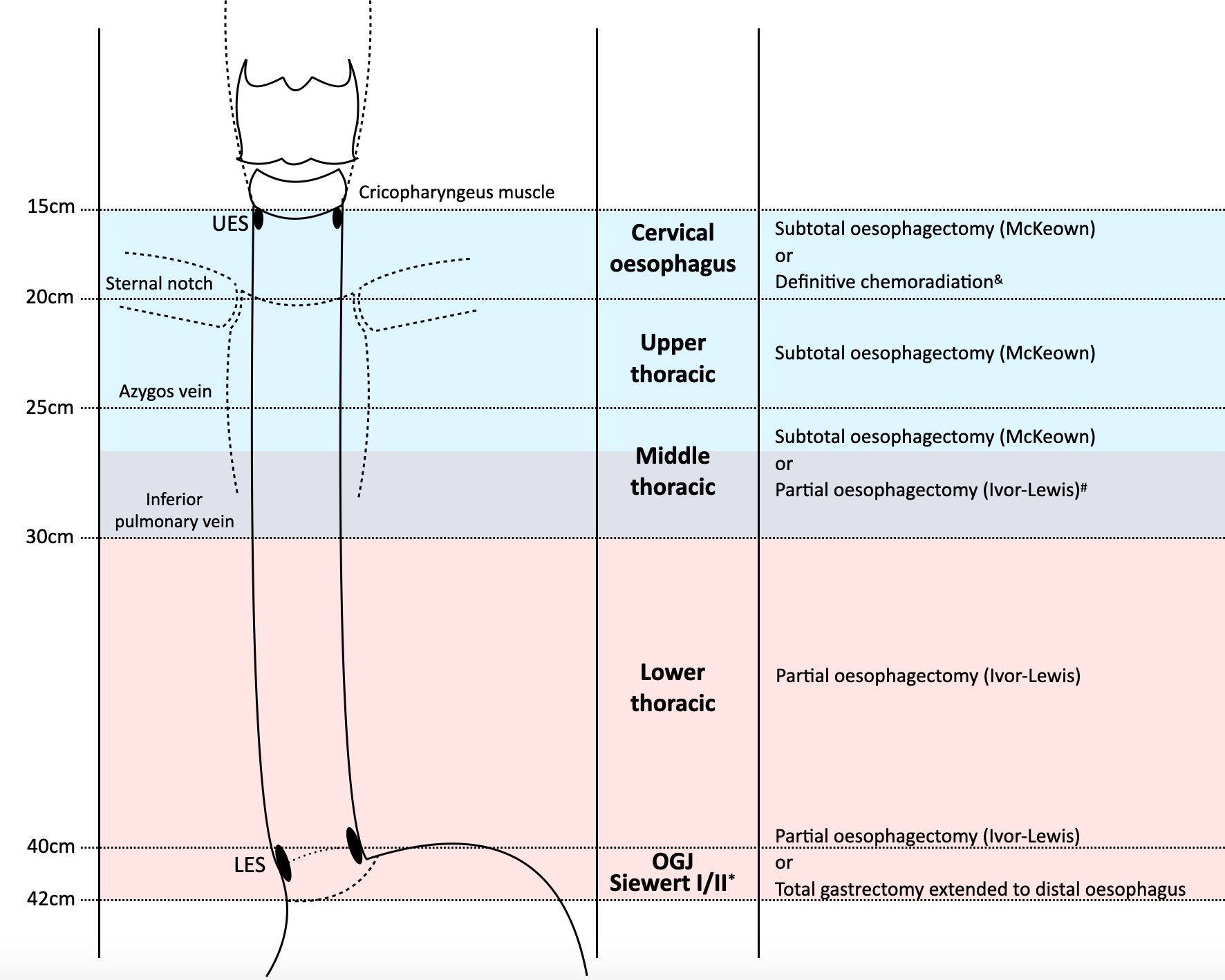
Introduction Oesophageal cancer ranks seventh in terms of incidence and sixth in mortality overall, being responsible for one in every 18 cancer deaths in 2020 worldwide1. There are two main histological types: squamous cell carcinoma and adenocarcinoma. The overall 5-year survival of patients diagnosed with oesophageal cancer is approximately 15%2. Apart from some areas in Asia, there is no screening programme worldwide. Hence, patients often present with advanced disease stage and cure is seldom possible. Some 50-60% of patients can be offered treatment with curative intent including surgical and non-surgical modalities3. Disease stage, patient’s fitness/frailty and expertise of the multidisciplinary team guide decision making. Anatomy of the oesophagus (figure 1)
The evolution of surgical treatment for achalasia: from experimental evidence to real-world impact
Luigi Marano, MD, PhD, Natale Di Martino, MD
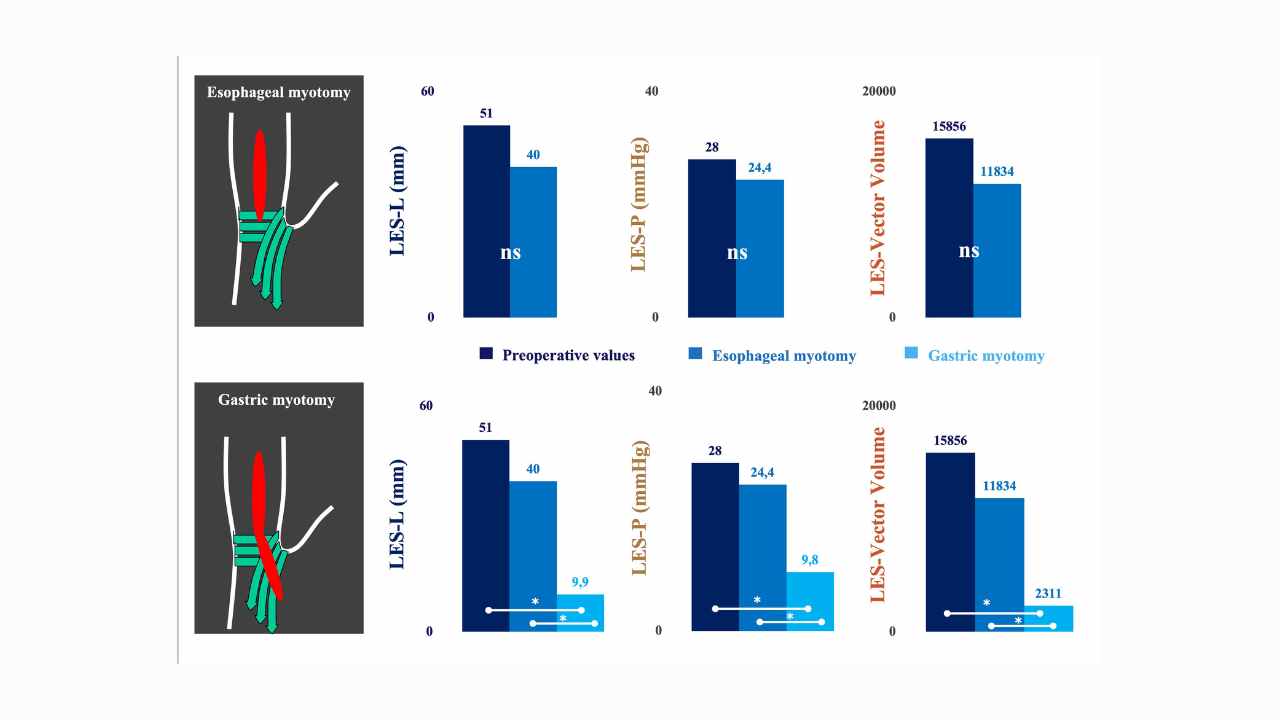
The optimal length of myotomy Achalasia, an immune-mediated disorder of oesophageal dysmotility, is characterized by impaired relaxation at the oesophagogastric junction (OGJ) and the absence of peristalsis upon swallowing1. These pathological alterations culminate in a functional outflow obstruction at the OGJ, leading to inefficient transit of the food bolus and manifesting as symptoms of dysphagia and non-acid regurgitation2. Therapeutic interventions aim to disrupt the OGJ complex to facilitate passive bolus transit into the stomach, thereby alleviating symptoms and improving long-term quality of life. The primary objective of current therapeutic options is to achieve sustained relief of dysphagia while minimizing the risk of symptom recurrence. Standard treatments such as pneumatic dilation, laparoscopic Heller myotomy (LHM), and per-oral endoscopic myotomy (POEM) are employed to lower oesophageal sphincter (LOS) pressure, thereby enhancing oesophageal outflow dynamics and ameliorating symptoms3–5. These interventions represent frontline approaches in the management of achalasia, providing effective palliation by addressing the underlying pathophysiology of the condition. The surgical management of achalasia stands out as the most effective approach among available treatments, offering favourable short- and long-term clinical outcomes5,6,7. This efficacy is particularly pronounced with the adoption of minimally invasive techniques, which have now become the preferred treatment for patients with idiopathic achalasia. However, despite the advantages of laparoscopic myotomy, it is important to acknowledge inherent limitations associated with the laparoscopic approach, such as bi-dimensional vision and restricted range of movement, which may impact on surgical precision. Recently, robotic technology has emerged as a promising alternative, with proponents suggesting its potential to reduce intraoperative oesophageal perforation rates and improve postoperative quality of life following Heller myotomy8. This potential enhancement is primarily attributed to the three-dimensional visualization and enhanced surgical dexterity offered by robotic systems.

International Bariatric Club BJS Lecture 2024: Towards sustainability in the operating room and the future of single use instruments in bariatric surgery
Robin Blackstone presents her BJS Lecture "Towards sustainability in the operating room and the future of single use instruments in bariatric surgery" from the 5th World Congress of the International Bariatric Club (IBC) held at Oxford University from 17-19 September 2024.
Copied!
