BJS Academy>Cutting edge blog>Author response: Ass...
Author response: Assessment of nodal staging and risk factors for nodal involvement in gallbladder cancer
Anita Balakrishnan
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Petros Barmpounakis
Cambridge Clinical Trials Unit—Cancer Theme, Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK; Department of Statistics, Athens University of Economics and Business, Athens, Greece
Nikolaos Demiris
Cambridge Clinical Trials Unit—Cancer Theme, Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK; Department of Statistics, Athens University of Economics and Business, Athens, Greece
Bodil Andersson
Department of Surgery, Lund University, Skane University Hospital, Lund, Sweden
Alejandro Brañes
Department of Hepatopancreatobiliary Surgery, Hospital Sotero del Rio, Puente Alto, Chile
Xavier de Aretxabala
Department of Digestive Surgery, Hepato-Pancreato-Biliary Surgery Unit, Surgery Service, Gallbladder Consortium Chile, Sotero del Rio Hospital and Clinica Alemana, Santiago, Chile
Malin Sternby Eilard
Transplantation Centre, Sahlgrenska University Hospital, and Department of Surgery, Institute of Clinical Sciences, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
Paul Gibbs
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Simon J F Harper
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Emmanuel L Huguet
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Asif Jah
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Vasilis Kosmoliaptsis
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Javier Lendoire
Department of Surgery, University of Buenos Aires, Hospital Dr Cosme Argerich, Buenos Aires, Argentina
Siong S Liau
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Shishir Maithel
Division of Surgical Oncology, Lurie Comprehensive Cancer Centre, Northwestern University, Chicago, USA
Jack L Martin
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Colin Noel
Gastrointestinal Surgery and Hepatopancreatobiliary Surgery, Department of Surgery, University of the Free State, Bloemfontein, South Africa
Raaj K Praseedom
Department of Hepatopancreatobiliary Surgery, Cambridge University Hospitals NHS Foundation Trust, University of Cambridge, Cambridge, UK; Department of Surgery, University of Cambridge, Cambridge, UK
Alejandro Serrablo
Department of Hepatopancreatobiliary Surgery, Miguel Servet University Hospital, Zaragoza, Spain
Volkan Adsay
Department of Pathology, Koç University Hospital, Istanbul, Turkey; Department of Pathology, Koç University Research Centre for Translational Medicine (KUTTAM), Istanbul, Turkey
the OMEGA Study Investigators
Related articles
Guest blog: Venous resection during pancreatoduodenectomy – there is still much to gain
J.V. Groen, Department of Surgery, Leiden University Medical Centre, Leiden, J.V.Groen@lumc.nl N. Michiels, Department of Surgery, Leiden University Medical Centre, Leiden, N.Michiels@lumc.nl J.S.D. Mieog, Department of Surgery, Leiden University Medical Centre, Leiden, J.S.D.Mieog@lumc.nl
IMPORTANCE
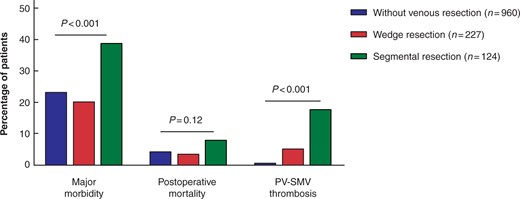
The use of venous resection (portal or superior mesenteric vein [PV-SMV]) during pancreatoduodenectomy is increasing.1-4 In a recent international survey, we found that most pancreatic surgeons prefer a segmental resection with primary anastomosis over a partial wedge resection, because of a lower perceived risk of complications.5 The impact of the type of venous resection (wedge or segmental) on postoperative morbidity and survival is poorly understood in current literature.
QUESTION
Video: Intervention versus surveillance in patients with common bile duct stones detected by intraoperative cholangiography
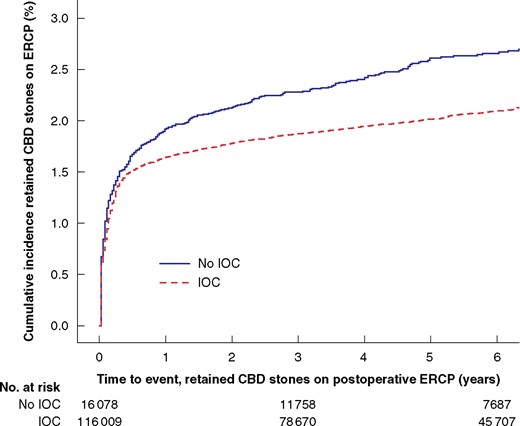
Each year 13 000 patients undergo cholecystectomy in Sweden, and routine intraoperative cholangiography (IOC) is recommended to minimize bile duct injuries. IOC plus an intervention to remove CBD stones identified during cholecystectomy was associated with reduced risk for retained stones and unplanned ERCP, even for the smallest asymptomatic CBD stones in this BJS study.
Video: Early postoperative arterial lactate concentrations to stratify risk of post-hepatectomy liver failure
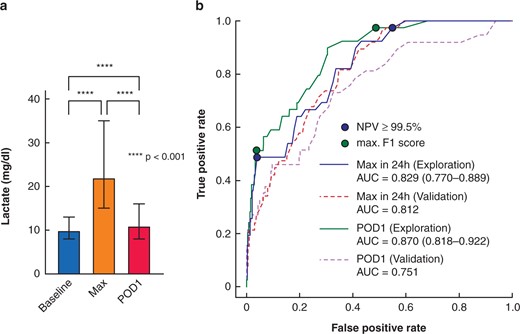
Post-hepatectomy liver failure (PHLF) represents the major determinant for death after liver resection. Early recognition is essential. Early postoperative lactate values are powerful, readily available markers for clinically relevant PHLF and associated complications after hepatectomy with potential for guiding postoperative care. This video explains the recent study published in BJS.
Copied!
