What's new
TOP ARTICLE
OF THE
MONTH

A view from the coffee room...How to retire gracefully: 10 commandments for surgeons

TestR-Author response: Ligation of intersphincteric fistula tract (LIFT) for trans-sphincteric cryptoglandular anal fistula: long-term impact on faecal continence
van Oostendorp JY1,2, Verkade C3, Han-Geurts IJM2, van der Mijnsbrugge GJH2, Wasowicz-Kemps3, Zimmerman DDE3

R- test
Kristine Hagelsteen, MD PhD

Rev test
Kristine Hagelsteen, MD PhD, Chris Mathieu

Science in a flash: pain, anxiety, stress and sleep disturbances among surgical patients
Jetske Marije Stoop, Markus Klimek, MD, PhD, DEAA, EDIC, FESAIC

Author response: Assessment of nodal staging and risk factors for nodal involvement in gallbladder cancer
Anita Balakrishnan, Petros Barmpounakis, Nikolaos Demiris, Bodil Andersson, Alejandro Brañes, Xavier de Aretxabala, Malin Sternby Eilard, Paul Gibbs, Simon J F Harper, Emmanuel L Huguet, Asif Jah, Vasilis Kosmoliaptsis, Javier Lendoire, Siong S Liau, Shishir Maithel, Jack L Martin, Colin Noel, Raaj K Praseedom, Alejandro Serrablo, Volkan Adsay, the OMEGA Study Investigators

A tribute to Paul Sugarbaker: the father of cytoreductive surgery
Aditi Bhatt MS, MCh, Brendan J. Moran MD, Marcello Deraco MD, Naoual Bakrin MD PhD, Joel Baumgartner MD, Vahan Kepenekian MD, PhD, Alvaro Arjona Sanchez MD, Vivek Sukumar MS, MCh, Kiran Turaga MD, MPH, Laurent Villeneuve MBE, PhD, Shigeki Kusamura MD, PhD, Olivier Glehen MD, PhD
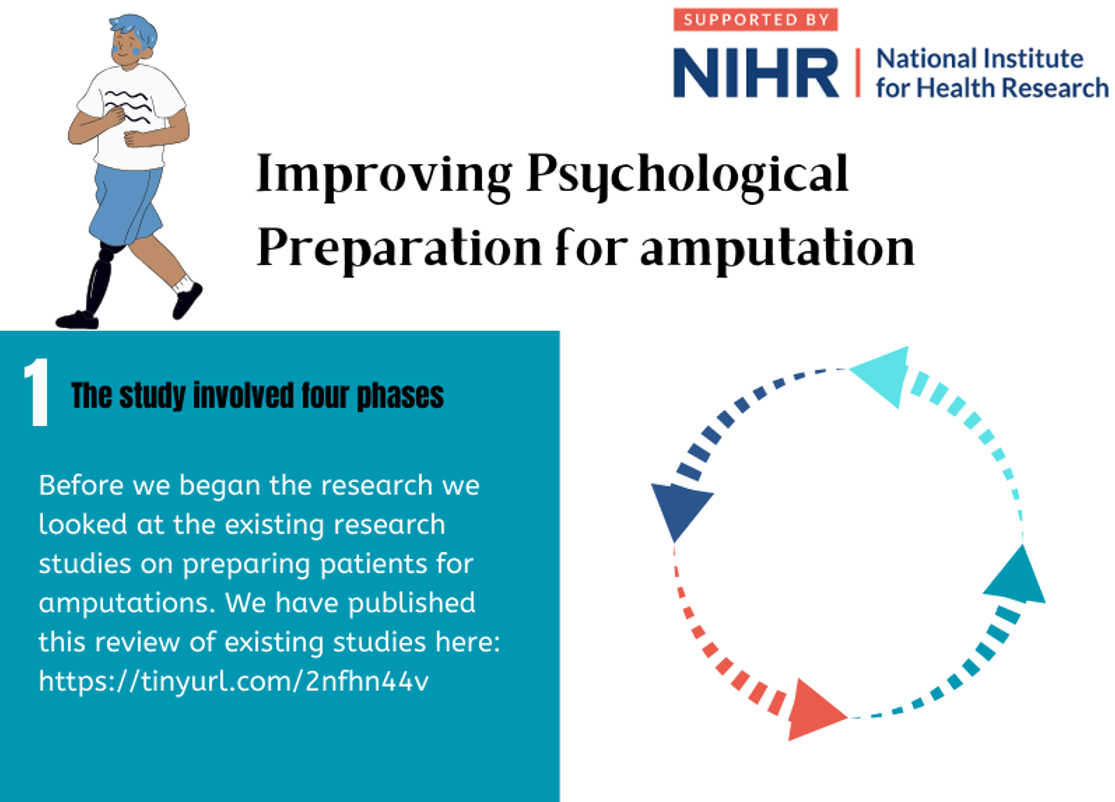
Improving the pre-operative psychological preparation of amputation patients
Dr Esmée Hanna
2025 Association of Surgeons in Training BJS Prize: Open repair vs endovascular repair in connective tissue disease patients with thoracoabdominal aortic pathologies - a systematic review & meta-analysis
JOIN
BJS Academy
Join BJS Academy And Receive Our Latest News And Updates.
About

BJS Academy is an online educational resource for current and future surgeons. It serves as the home for all things relating to the BJS Foundation as well as produces content, both original and in conversation with material published in the BJS Journals.
BJS Academy was founded as a part of the charitable activity of BJS Foundation, which owns and operates the following.

A celebration of excellence in surgical science, the BJS Award recognises a discovery, innovation or scientific study that has changed clinical practice. Awarded every two years, this international accolade gives an exceptional individual the recognition they richly deserve.
Academy content is comprised of five distinct sections: Continuing surgical education, Young BJS, Cutting edge, Scientific surgery and Surgical news.

BJS Institute provides formal certified online surgical courses to surgeons in training and established surgeons who wish to develop their skills in surgical writing and publishing.

Championing a Partners collaborative approach, the Foundation offers two levels of partnership, each with their own unique benefits.